Many people believe psoriatic arthritis starts with skin symptoms. But that’s not always true. Some patients notice joint pain before any psoriasis develops. Morning stiffness is common. The joints feel heavy, tight, or slow to respond. Wrists, fingers, knees, and ankles may ache for months. Doctors may misdiagnose it as general wear-and-tear. Joint stiffness may come before any visible skin issues, which delays proper treatment and attention.
It doesn’t behave like other common joint diseases
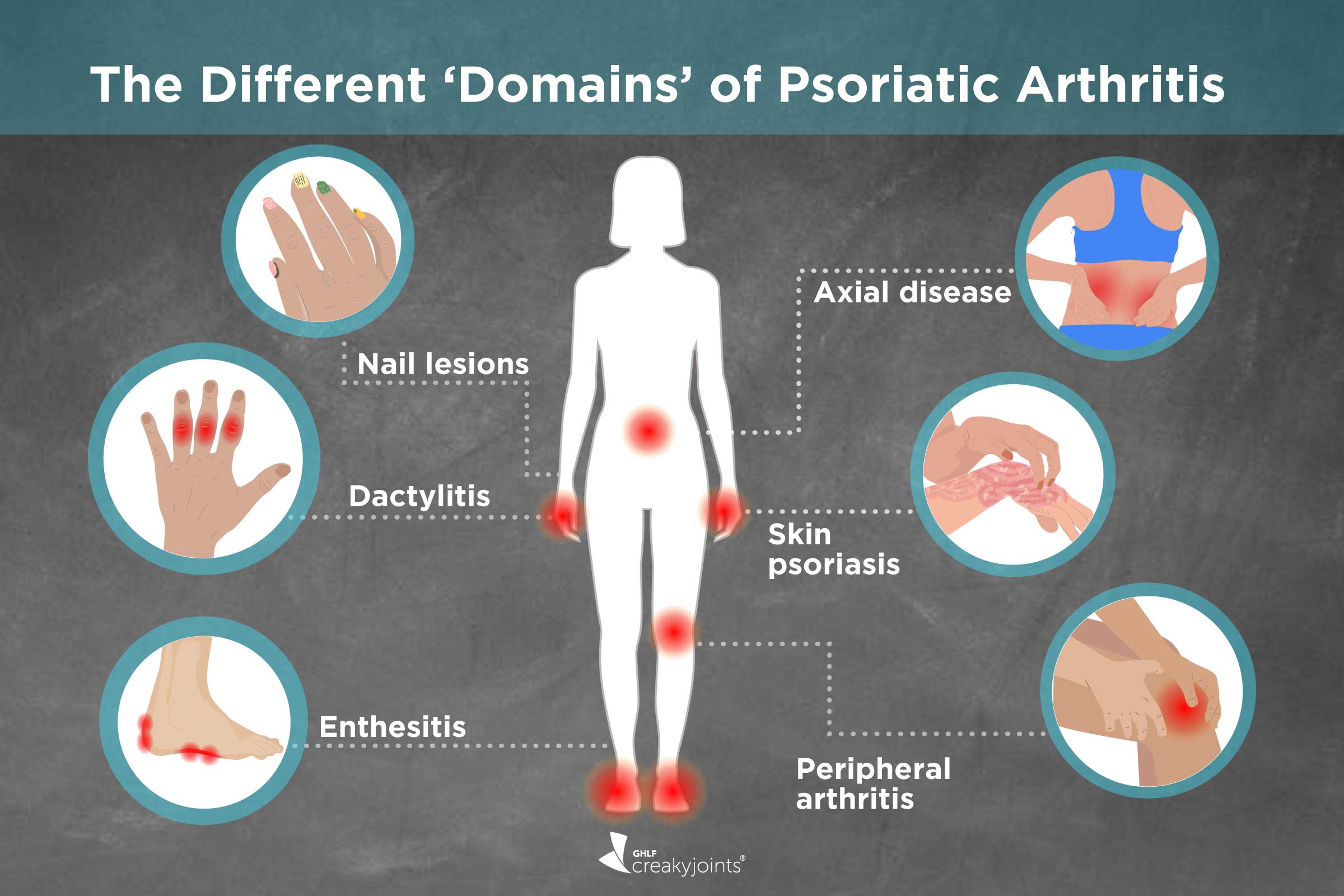
Psoriatic arthritis isn’t the same as rheumatoid or osteoarthritis. It doesn’t follow a single pattern. Some joints flare up while others stay calm. Fingers might swell unevenly. Symptoms shift over weeks or months. One day it’s your toes, the next it’s your lower back. It doesn’t behave like other common joint diseases, which is why it’s often misunderstood—even by patients.
Skin flares and joint pain don’t always appear together
The assumption is that skin and joint symptoms arrive at the same time. But many people have long periods where only one is active. A person may experience a skin flare but no joint pain. Or the opposite—intense joint stiffness without visible plaques. This disconnect leads people to doubt the diagnosis. Skin flares and joint pain don’t always appear together, even though they stem from the same immune system imbalance.
Nail changes can offer early clues before diagnosis
Nails often reveal what the joints don’t. Pitting, discoloration, or separation from the nail bed can appear early. These changes are easily dismissed as cosmetic. But they reflect inflammation beneath the surface. Around 80% of people with psoriatic arthritis have some nail involvement. Nail changes can offer early clues before diagnosis, especially when other signs are still mild.
Swelling may affect entire fingers or toes
Unlike other forms of arthritis, psoriatic arthritis can cause dactylitis. This means an entire digit swells—finger or toe—not just a single joint. It becomes red, tender, and sausage-like. The swelling doesn’t move from joint to joint. It lingers and limits movement. Swelling may affect entire fingers or toes and may be mistaken for injury or infection if unfamiliar.
Fatigue doesn’t always correlate with disease severity
Some days, the exhaustion is overwhelming. Not just from pain—but from systemic inflammation. The body feels drained even after rest. People describe it as bone-deep tiredness. It may arrive even when the joints feel fine. Fatigue doesn’t always correlate with disease severity, but it affects daily life profoundly.
Psoriatic arthritis can damage joints without causing severe pain
This condition doesn’t always present with high levels of pain. Sometimes the damage happens silently. People continue daily activities, unaware their joints are deteriorating. Imaging reveals erosion, but the person feels little discomfort. Psoriatic arthritis can damage joints without causing severe pain, which makes early screening vital.
It can affect the spine and pelvis without skin signs
Some people with psoriatic arthritis develop axial disease. This targets the spine, sacroiliac joints, and pelvis. They feel back stiffness, especially in the morning or after rest. These symptoms mimic mechanical back pain. But unlike regular back pain, it improves with activity. It can affect the spine and pelvis without skin signs—so it’s often mistaken for a strained muscle or poor posture.
Eye inflammation may occur alongside joint symptoms
Psoriatic arthritis isn’t confined to the skin or joints. Some patients develop uveitis—an inflammation of the middle eye layer. This causes redness, light sensitivity, and blurred vision. It’s painful and may recur. Eye inflammation may occur alongside joint symptoms, and ignoring it could risk long-term damage.
It affects mental health through chronic discomfort and isolation
The physical symptoms are visible. The emotional toll isn’t. Living with an unpredictable illness changes routines, work, and relationships. People withdraw to avoid explaining their condition. Flare-ups interrupt plans. Anxiety and depression become common companions. It affects mental health through chronic discomfort and isolation—though few talk openly about it.
Psoriatic arthritis is not simply “bad psoriasis”
Many people, including patients, confuse the two conditions. Psoriasis affects the skin. Psoriatic arthritis is a separate, complex disease. The immune pathways differ. Treatments vary. Not everyone with psoriasis will develop arthritis, and not all arthritis sufferers have skin plaques. Psoriatic arthritis is not simply “bad psoriasis”—it’s a multi-system autoimmune disorder with its own challenges.
Some people experience severe symptoms with only mild skin issues
A person with minor psoriasis may have significant joint disease. Their elbows may be clear. Their knees pain-free. But fingers or back may suffer deeply. Doctors often overlook this if the skin isn’t flaring. Some people experience severe symptoms with only mild skin issues, making diagnosis harder to reach.
Diagnosis often takes longer than it should
This disease hides behind other names. “Tendonitis.” “Back strain.” “Stress.” Patients bounce between doctors. They try painkillers or physical therapy. Blood tests are often normal. No single marker confirms the disease. Diagnosis often takes longer than it should, especially when symptoms don’t match classic expectations.
Enthesitis is pain where tendons attach to bone
Psoriatic arthritis often inflames the spots where ligaments or tendons meet bone. The Achilles tendon. The bottom of the foot. The outer elbow. These spots become sore and tender. Walking or gripping becomes painful. Enthesitis is pain where tendons attach to bone—and it’s a hallmark of psoriatic arthritis.
Medication choices vary based on symptom location
There’s no one-size-fits-all drug for psoriatic arthritis. Some meds target joints. Others target skin. Biologics may help both. Some patients need a combination. Side effects differ. Monitoring is critical. Medication choices vary based on symptom location and must be adjusted over time.
Early treatment can prevent permanent joint damage
Delays in treatment allow inflammation to erode cartilage and bone. Over time, joints lose shape and function. This damage can’t be reversed. But early intervention can stop progression. Early treatment can prevent permanent joint damage and preserve mobility well into old age.
Flare-ups don’t always follow a pattern
One month, everything feels stable. The next, pain and swelling return. Triggers are unclear. Stress. Weather. Infection. Overuse. Even rest can sometimes provoke symptoms. Flare-ups don’t always follow a pattern, which frustrates patients seeking predictability in an unpredictable condition.
Regular movement is essential, but must be balanced
Exercise supports joint health and reduces stiffness. But too much causes fatigue and inflammation. Balance is key. Gentle stretches, swimming, and walking work well. Rest is also necessary. Regular movement is essential, but must be balanced carefully based on daily symptoms.
Living with psoriatic arthritis requires constant adjustment
This condition changes over time. What works now may not work later. Pain moves. Energy shifts. Plans change. Diet, sleep, stress—all influence symptoms. Living with psoriatic arthritis requires constant adjustment, flexibility, and honest self-reflection without self-blame.
Source: Rheumatologist in Dubai / Rheumatologist in Abu Dhabi
