Vasculitis, a name that evokes a sense of complexity and mystery, is a group of rare diseases that share a common and destructive characteristic: inflammation of the blood vessels. This inflammation, which can affect arteries, veins, and capillaries, can lead to a host of problems, from a simple rash to life-threatening organ damage. The sheer variety of vasculitic diseases, each with its own set of triggers, symptoms, and affected vessels, makes diagnosis and treatment a formidable challenge for even the most experienced clinicians. It is not a single condition but a spectrum of disorders where the body’s own immune system, for reasons not always understood, turns against its vital circulatory network.
The sheer variety of vasculitic diseases, each with its own set of triggers, symptoms, and affected vessels, makes diagnosis and treatment a formidable challenge.
The root cause of vasculitis often lies in a malfunction of the immune system. In a healthy body, the immune system’s job is to identify and destroy foreign invaders like bacteria and viruses. In vasculitis, this system becomes confused and mistakenly attacks the cells lining the blood vessels. This attack triggers an inflammatory response that can cause the vessel walls to thicken, narrow, or even close completely, obstructing the flow of blood to organs and tissues. The resulting damage can lead to a deprivation of oxygen and nutrients, a condition known as ischemia, which can cause severe pain and tissue death. The body’s misguided defense mechanism is the central problem that all treatments must address.
The body’s misguided defense mechanism is the central problem that all treatments must address.
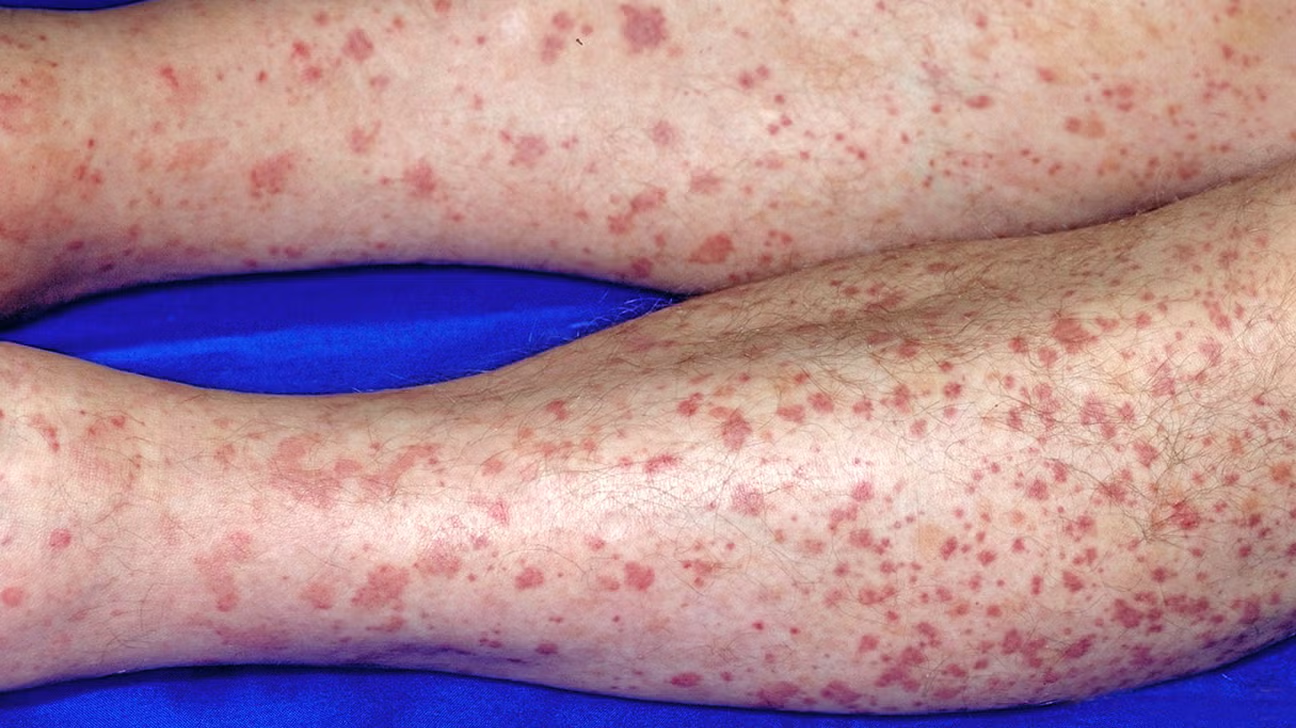
Symptoms of vasculitis can be as diverse as the diseases themselves, making them difficult to pin down. A patient might present with a seemingly minor symptom, like a red or purple rash on the legs, which is actually a sign of inflammation in the tiny capillaries of the skin. Others may experience more systemic and severe symptoms, such as fever, fatigue, weight loss, and joint pain, which can easily be mistaken for a host of other conditions. The symptoms are directly tied to the location and size of the affected blood vessels. For instance, if large arteries leading to the head are inflamed, a person might experience severe headaches and vision problems. If the tiny vessels in the kidneys are involved, it could lead to kidney failure without any external signs until the disease is advanced.
A patient might present with a seemingly minor symptom, like a red or purple rash on the legs.
Diagnosing vasculitis is a detective-like process that requires careful attention to detail. A doctor will typically start with a thorough medical history and a physical examination, looking for a combination of symptoms that point toward a vasculitic disorder. Blood tests are a crucial next step, as they can reveal markers of inflammation and the presence of specific antibodies that are associated with certain types of vasculitis. However, blood tests alone are often not enough. A definitive diagnosis frequently requires a biopsy of the affected tissue or blood vessel. A small sample is removed and examined under a microscope for signs of inflammation and damage. This definitive evidence is often the final piece of the puzzle that allows a doctor to confidently diagnose vasculitis and determine its specific type.
A definitive diagnosis frequently requires a biopsy of the affected tissue or blood vessel.
Treatment for vasculitis is highly dependent on the type and severity of the disease. The primary goal of treatment is to reduce inflammation and suppress the overactive immune system to prevent further damage to organs. The cornerstone of treatment for most forms of vasculitis is a class of drugs known as corticosteroids, such as prednisone. These powerful anti-inflammatory medications can quickly bring the disease under control, particularly in its acute phase. However, due to their side effects with long-term use, they are often used in high doses initially and then tapered down as other medications take effect.
The primary goal of treatment is to reduce inflammation and suppress the overactive immune system.
Beyond corticosteroids, other immunosuppressant drugs are often used to maintain remission and allow for the reduction of steroid dosage. These medications, such as cyclophosphamide, methotrexate, and azathioprine, work by inhibiting the immune system’s function, thereby preventing it from attacking the blood vessels. The choice of which immunosuppressant to use depends on the specific type of vasculitis and the patient’s overall health. In recent years, newer biologic drugs, which target specific parts of the immune system, have also shown great promise in treating certain forms of vasculitis, offering a more targeted approach with potentially fewer side effects.
The choice of which immunosuppressant to use depends on the specific type of vasculitis.
Managing vasculitis is not a short-term affair; it often requires a long-term commitment from both the patient and the medical team. After the initial treatment phase, the focus shifts to maintaining remission, which means keeping the disease in a quiet state and preventing it from flaring up. This involves regular monitoring through blood tests, urine tests, and sometimes imaging studies to ensure that the disease activity remains low. It is a balancing act, as doctors must weigh the benefits of continued medication against the potential for side effects, particularly with long-term use.
Managing vasculitis is not a short-term affair; it often requires a long-term commitment.
Living with vasculitis is not just about taking medication; it also involves lifestyle adjustments. Patients are often advised to adopt a healthy diet, get regular exercise, and avoid smoking, all of which can support overall vascular health. Learning to recognize the early signs of a flare-up is also critical, as prompt medical attention can often prevent a minor problem from escalating into a serious one. This involves paying close attention to one’s body and communicating openly with the medical team. The patient becomes an active participant in their own care, a partner in the fight against the disease.
The patient becomes an active participant in their own care, a partner in the fight against the disease.
The psychological burden of living with a chronic, unpredictable disease should not be underestimated. The uncertainty of a flare-up, the side effects of medication, and the impact on daily life can be overwhelming. Support groups and counseling can provide invaluable emotional support and practical advice from others who are navigating a similar journey. A holistic approach to care, which addresses both the physical and mental aspects of the disease, is essential for a person to live a full and productive life.
The psychological burden of living with a chronic, unpredictable disease should not be underestimated.
In conclusion, vasculitis is a complex and often misunderstood group of diseases that require a tailored and long-term approach to treatment. It is a journey that involves careful diagnosis, a combination of potent medications, and a commitment to lifestyle changes. The goal is to not only control the disease but to restore a sense of normalcy and quality of life for those affected.
